Recovery After UFE

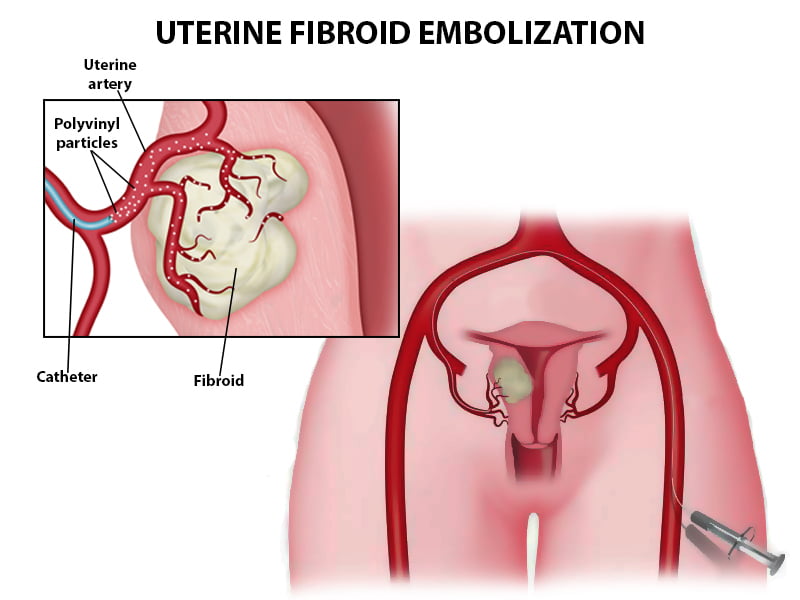
The procedure of uterine fibroid embolization is used to remove or shrink uterine fibroids. A thin, flexible tube (catheter) was inserted into blood vessels in both of your upper thighs by your doctor. The doctor next injected microscopic particles into your fibroids through the catheter to prevent them from absorbing blood.
Every day, you should expect to feel better. However, you may become exhausted rapidly and require pain medication for several days. It may take 7 to 10 days for you to fully recover.
After uterine fibroid embolization, many women experience mild to severe cramping for many days. For the next 4 to 5 days, you may experience minor nausea and a slight fever. For several weeks, some women experience vaginal bleeding or a greyish or brownish vaginal discharge. These are all common side effects.
It’s possible that your next few menstrual cycles will be heavier than usual. After the operation, some women continue to discharge tissue for up to three months.
Make sure you don’t do any hard lifting for at least a week.
Caring for yourself at home
Activity
- When you’re exhausted, take a break. You will be able to recuperate faster if you get adequate sleep.
- Every day, try to go for a walk. Begin by going for a longer stroll than you did the day before. Gradually increase your walking time. Walking improves blood circulation and aids in the prevention of pneumonia and constipation.
- For 1 week, avoid lifting anything that would make you strain.
- Avoid strenuous activities for 4 weeks, such as biking, jogging, weightlifting, and aerobic exercise.
- You may shower. Do not take a bath for a few days or until your doctor tells you it is okay.
- You may have some vaginal bleeding. Do not use tampons.
- Your doctor will tell you when you can have sex again.
Diet
- You can eat your normal diet. If your stomach is upset, try bland, low-fat foods like plain rice, broiled chicken, toast, and yogurt.
- Drink plenty of fluids.
- Right after surgery, you may find that your bowel movements are irregular. Constipation and bowel straining should be avoided. You should consider taking a fiber supplement on a daily basis. Ask your doctor about using a mild laxative if you haven’t had a bowel movement in a few days.
Medicines
- Your doctor will tell you when you can restart your medicines.
- If the doctor gave you a prescription medicine for pain, take it as prescribed
- If your doctor prescribed antibiotics, take the full course of antibiotics as directed.
Other instructions
- Avoid any clothes that pressuring your belly for a few days.
- Use a heating pad on your belly to help with the pain.
Follow-up care is a key part of your treatment and safety.
When should you call for help?
Call 911 anytime you think you may need emergency care. For example, call if:
- You passed out (lost consciousness).
- You have chest pain, are short of breath, or cough up blood.
Call your doctor or nurse call line now or seek immediate medical care if:
- You have bright red vaginal bleeding that soaks one or more pads in an hour, or you have large clots.
- You are sick to your stomach or cannot drink fluids.
- You have vaginal discharge that has increased in amount or smells bad.
- You have signs of infection, such as:
- Increased pain, swelling, warmth, or redness.
- A fever.
- You have signs of a blood clot in your leg (called a deep vein thrombosis), such as:
- Pain in your calf, back of the knee, thigh, or groin.
- Redness and swelling in your leg or groin.
- You have pain that does not get better after you take pain medicine.
- You are bleeding from the area where the catheter was put in your artery.
- You have a fast-growing, painful lump at the catheter site.
Watch closely for any changes in your health, and be sure to contact your doctor or nurse’s call line if you have any problems.
Recovery After Varicose Vein Surgery
Your varicose veins were surgically removed during the surgery. Here are some things you may take to speed up your recovery after surgery.
Home care
Recommendations for taking care of yourself at home include the following:
- For the first 2 weeks after surgery, avoid standing for long periods. Also, avoid heavy lifting.
- Keep your legs raised when you’re sitting or lying down.
- Starting the day after surgery, begin a regular walking regimen. Start with a few minutes of walking and gradually increase to 5 minutes at a time. Increase to 15 to 20 minutes at a time, 2 to 3 times per day, gradually.
- Wear bandages or elastic stockings as instructed by your doctor. Move your feet back and forth and in circles while sitting to keep your circulation flowing.
- Ask your doctor when you can resume driving and working.
When to call your doctor
Call your doctor right away if you have any of the following:
- Severe bleeding, redness, or drainage
- Development of an ulcer (sore)
- Legs or feet numbness or tingling
- Leg swelling or pain that is getting worse
- Fever, shaking, or chills
- Shortness of breath or chest pain
Updated on Jan 18, 2025 by Dr. George Bolotin (Vein & Vascular Specialist) of Vein & Vascular Medical Care
Vein & Vascular Medical Care
4209 Ave U, Suite A.
Brooklyn, NY 11234
(347) 934-9068
Vein & Vascular Medical Care
869 E Tremont Ave
Bronx, NY 10460
(929) 447-4563